If you haven’t looked into individual coverage health reimbursement arrangements (ICHRAs) that took effect this year, consider putting it on your to-do list; it gives you an option for reining in escalating health insurance costs for your employees.
Federal rules implementing the new benefit took effect on January 1. Under ICHRAs, instead of offering your employees a traditional group health insurance plan, you can offer them money to buy their own coverage in the individual market.
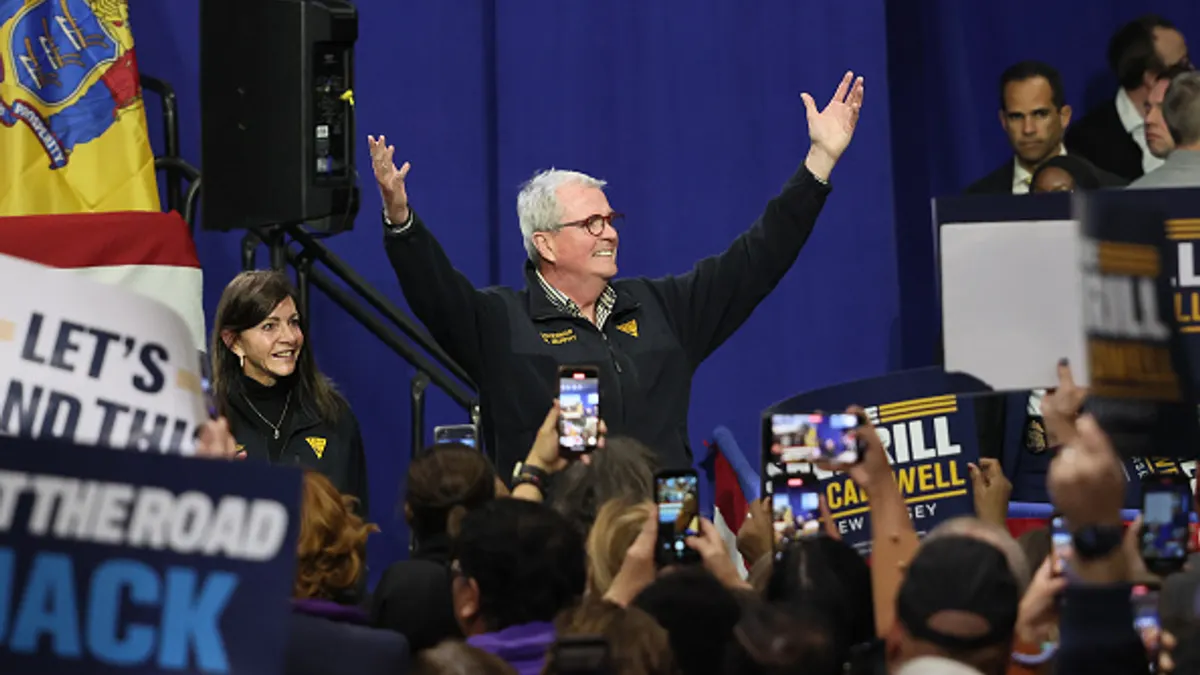
The federal government is touting the program as a way to spend less time managing insurance risk so you can focus on your core competencies, Bruce Gillis, compliance lead for Businessolver, a benefits administrator, said last week in a CFO.com webinar.
"That is 100% the value statement behind the program," said Gillis, who recently attended a meeting on the program with administration officials in Washington.
The program was created as a federal regulatory initiative in 2017 and could reach as many as 11 million employees once it’s fully implemented, said Brady Young, president and CEO of Strategic Risk Solutions.
Over the past two decades, health insurance costs have risen at three times the pace of inflation, and now the typical cost of family coverage is more than $20,000 a year per employee, making it one of the biggest line items in organizations’ budgets. "Everyone’s desperate to rein in costs," Young said.

With the program, you can make it a competitive selling point in a tight labor market if you’re trying to attract part-time workers. Unlike traditional group plans, ICHRAs are an eligible benefit to part-timers and even temporary workers if you choose to offer it to them.
"An employer could say, 'You know, we’re struggling with this part-time population that’s not traditionally eligible for benefits,'" said Gillis. "'We can offer an ICHRA and provide some level of funding to make that job more attractive.'"
Flexible rules
The rules give you flexibility on how much to set aside for each employee. Nationwide, the average is $387 a month, said Chini Krishnan, president and CEO of GetInsured, an insurance market shopping portal.
Whatever amount you decide, it has to be consistent across classes of employment. That means you have to offer the same amount to any employee who’s, say, full-time vs. part-time, salaried vs. wage-earning, and so on.
There are two exceptions to this. You can offer more for older workers and those with more dependents.
You can also offer different amounts based on where the employees are located, because coverage costs vary widely by geography.
"A 40-year old in Minnesota differs from one in Wyoming, so the amount of contribution required to be affordable will vary," said Gillis. "It may take $350 in Minnesota but it will take $425 in Wyoming."
Employees in control
Once you set your amounts, it’s up to employees to shop around for coverage. You have to be prepared to help them, though; the rules require you to offer them decision support by making resources and guidance available to them.
If you offer a traditional group plan and want to switch to an ICHRA, you have to let your employees know at least 90 days in advance.
It’s natural for employees to express concern over the change, the benefits specialists said, because it puts responsibility on their shoulders. But once they see how it puts them in control of their benefit, they should embrace it, said Krishnan.
"When they understand they can apply to any plan they want, they like that," he said.
Eligibility is limited to people who don’t have a group coverage plan available to them. So, if you have employees who are eligible for group coverage through a spouse, for example, they would not be able to participate.
"At the end of the day, healthcare inflation is not going away," said Krishnan. "The question we’re all confronted with is, how do you make it work?"
Revolutionizing Employer Risk: What CFOs Need to Know About the New HRAs was sponsored by Businessolver and Argyle Group.